Introduction
Resistance to covalent (ibrutinib, acalabrutinib and zanubrutinib) and non-covalent BTK inhibitors (pirtobrutinib) is an emerging clinical challenge. DZD8586 was designed as a full blood-brain barrier (BBB) penetrable LYN/BTK dual inhibitor. Preclinical study suggested DZD8586 has a good selectivity against other TEC family kinases (TEC, ITK, TXK, BMX). DZD8586 inhibits BTK-dependent and BTK-independent BCR signaling pathways by targeting LYN and BTK, which could potentially overcome resistance to both covalent and non-covalent BTK inhibitors for the treatment of CLL and MCL, as well as DLBCL. Two phase 1 clinical studies are ongoing in patients with relapsed or refractory (r/r) B-NHL to assess safety, pharmacokinetics (PK), pharmacodynamics (PD) and anti-tumor efficacy of DZD8586.
Methods
TAI-SHAN1 (NCT05844956; CTR20220558) and TAI-SHAN5 (NCT05824585) are phase 1 dose escalation and expansion studies in patients with r/r B-NHL. Both studies have similar dose escalation strategies. Patients who progressed following or intolerant of prior systemic therapy were enrolled. Pooled safety and efficacy analysis was performed. In addition, modulation of PD biomarkers was also evaluated. Tumor responses were investigator assessed according to Lugano 2014, IPCG 2005, or iwCLL 2018, as appropriate.
Results
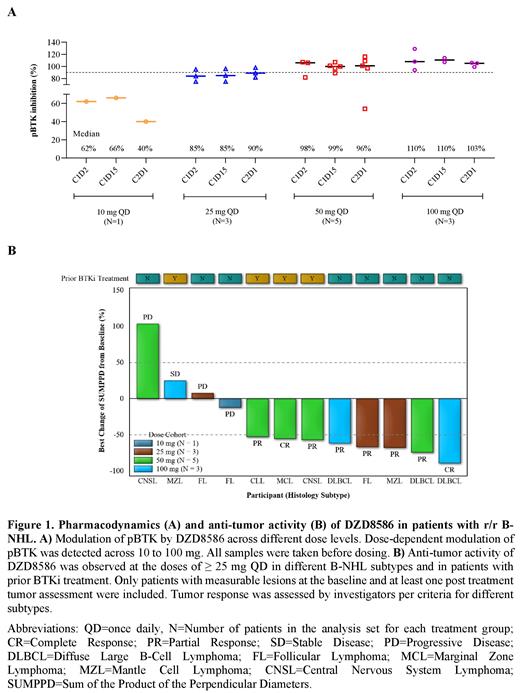
As of June 15, 2023, 17 patients with r/r B-NHL have been enrolled and received DZD8586 at doses ranging from 10 to 100 mg once daily (QD) (10 mg, n=1;25 mg, n=4;50 mg, n=7;100 mg, n=5). The median age was 61 years, 71% were male, and 53% had an ECOG PS of 1. Histological subtypes included CLL, SCNSL, DLBCL, MCL, FL and MZL. The median number of prior therapies was 3 (range 2 - 8). All patients received prior chemotherapy and anti-CD20 therapy. Six patients, including 1 CLL, 2 MCL, 1 MZL, 1 SCNSL and 1 DLBCL had received prior treatment with covalent BTK inhibitors.
DZD8586 was well tolerated across the doses investigated. Drug-related treatment emergent adverse events (TEAEs) reported in > 2 patients included thrombocytopenia (10/17), neutropenia (5/17), and upper respiratory tract infection (3/17). The most common ≥ grade 3 TEAE was thrombocytopenia (3/17, all at 100 mg). Other ≥ grade 3 TEAEs, including neutropenia, drug eruption and upper respiratory tract infection, were each reported by one patient. Bleeding, atrial fibrillation, and arthralgia were not reported. Grade 1 diarrhoea was reported in one patient. The maximum tolerated dose was defined as 100 mg QD.
All these TEAEs were reversible after dose interruption and/or with supportive care. The longest duration on treatment was 10+ months.
Among 13 patients treated at doses ≥ 25 mg QD with at least one tumor assessment, the objective response rate (ORR) was 9/13 (69.2%). Responses were observed across different histological subtypes (1/2 in SCNSL; 4/5 in DLBCL; 1/2 in FL; 1/1 in MCL, 1/2 in MZL and 1/1 CLL carrying C481S mutation). Among the 5 evaluable BTKi treated patients, tumor responses were observed in 3 patients. The longest duration of response (DoR) was 6.4+ months, and the patient was still ongoing with DZD8586 treatment and responding.
PK was generally dose-proportional across the dose ranges of 10 to 100 mg. DZD8586 was absorbed with median t max 1.5 hours, and eliminated with mean terminal half-life of ~18 hours. Accumulation of about two folds in AUC was noted at steady state following once daily dosing. Dose dependent pBTK modulation in whole blood cells was detected, and at the doses ≥ 25 mg, sustained pBTK inhibition was observed. The unbound CSF-to-plasma concentration ratio (K puu,CSF) was 1.2 from one CNSL patient with available CSF samples, suggesting excellent CNS penetration of DZD8586 in humans.
Conclusion
In the preliminary pooled analysis of two ongoing phase 1 trials, DZD8586 has encouraging anti-tumor activity and safety in heavily pre-treated B-NHL patients. The combination of BBB penetration, dual inhibition of LYN/BTK and potential to overcome C481S mutant CLL and other covalent BTKi resistant lymphomas suggest this may be a useful agent. Updated data will be presented at the meeting.
Disclosures
Bai:Dizal Pharmaceutical: Current Employment. Fang:Dizal Pharmaceutical: Current Employment. Liu:Dizal Pharmaceutical: Current Employment. Cheah:BMS: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; BeiGene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; TG therapeutics: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Lilly: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Gilead: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Dizal: Consultancy, Honoraria; AbbVie: Research Funding; Roche: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: TRAVEL, ACCOMMODATIONS, EXPENSES, Research Funding; AstraZenecca: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Ascentage Pharma: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Menarini: Consultancy, Honoraria; Genmab: Consultancy, Honoraria; MSD: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal